That persistent ache in your hand, the tingling sensation in your fingers, the stiffness that makes it difficult to grip a coffee mug, or the lingering pain from a sprained wrist can be more than just an inconvenience. Hand pain and wrist pain can significantly impact your daily life, making simple tasks feel frustrating and difficult. We understand that finding effective relief is key to restoring a pain-free and active lifestyle.
At Kansas City Orthopaedic Institute (KCOI), our dedicated team of orthopedics experts understands the intricate anatomy of the hand and wrist. We specialize in diagnosing and treating a wide range of conditions, from common overuse issues, like tendonitis, to complex injuries, such as fractures or dislocations. This blog post will serve as your comprehensive guide to understanding both the surgical and non-surgical treatment options available for hand pain and wrist pain, helping you navigate your path to recovery.
Understanding the Sources of Hand and Wrist Pain
The hand and wrist are marvels of anatomical engineering, composed of 27 bones, a complex network of ligaments, tendons, muscles, and nerves. Due to their frequent use and delicate structure, they are susceptible to a variety of conditions and injuries. The most common causes of hand pain and wrist pain include:
- Carpal Tunnel Syndrome: This is a condition where the median nerve, which runs from the forearm into the hand, becomes compressed at the wrist. It’s often caused by repetitive motions, forceful gripping, and exposure to high vibration activities. It can lead to tingling, numbness, weakness, and pain in the hand and fingers.
- Osteoarthritis: Often called “wear-and-tear” arthritis, it occurs when the cartilage that cushions the joints breaks down, leading to pain, stiffness, and loss of motion. It commonly affects the base of the thumb and the small joints of the fingers.
- Tendonitis and Tenosynovitis: Inflammation of a tendon or its sheath, often resulting from repetitive stress or overuse. A prime example is trigger finger, where a finger or thumb gets stuck in a bent position.
- Fractures: A break in one of the small bones of the hand or wrist, such as a wrist fracture from a fall.
- Sprained Wrist: A common injury that occurs when the ligaments supporting the wrist are stretched or torn, often from a fall, sports activity, or sudden impact. It can cause swelling, bruising, and pain with movement.
- Ganglion Cysts: Noncancerous, fluid-filled lumps that most often develop on the back of the wrist.
- De Quervain’s Tenosynovitis: Inflammation of the tendons on the thumb side of the wrist, causing pain with gripping or pinching motions.

Non-Surgical Treatment Options: The First Step to Relief
For many patients, especially those with mild to moderate symptoms, the journey to relief begins with conservative, non-surgical treatments. These approaches focus on reducing pain and inflammation, restoring function, and preventing further irritation. Our orthopedics team prioritizes these options whenever possible.
- Rest and Activity Modification: The simplest and often most effective treatment for overuse injuries. Avoiding or modifying activities that aggravate your symptoms can give the tissues time to heal.
- Physical or Occupational Therapy: A certified therapist can provide a personalized plan of exercises to improve strength, flexibility, and range of motion. They may also teach you ergonomic techniques to reduce strain during daily activities.
- Bracing or Splinting: Wearing a brace or splint can stabilize the hand or wrist, reducing stress on tendons and nerves and allowing inflamed tissues to rest and heal. This is particularly helpful for carpal tunnel syndrome, wrist tendonitis, or a sprained wrist.
- Medications: Over-the-counter anti-inflammatory medications, such as ibuprofen, can help manage pain and reduce swelling.
- Therapeutic Injections: A steroid injection can be a powerful tool to provide significant, though often temporary, relief from pain and inflammation. For conditions like carpal tunnel syndrome, therapeutic injections can reduce swelling around the compressed nerve. They are also effective for relieving the pain of arthritis and trigger finger.
When to Consider Surgery: A Targeted Approach
When non-surgical treatments no longer provide adequate relief, or in cases of severe conditions like a complex wrist fracture, surgery becomes the most effective option. Modern orthopedic surgery for the hand and wrist is highly specialized and often minimally invasive, with a focus on restoring long-term function and alleviating pain.
The expert surgeons at KCOA, our partner physician clinic, utilize the latest techniques to ensure the best possible outcomes for our patients. The following physicians constitute the hand and wrist team at KCOI, and specialize in surgical and non-surgical treatment for hands and wrists:
- Valerie Deardorff, MD
- Burrel Gaddy, Jr, MD
- Patrick Murray, MD
- Robert Sharpe, MD
- Kenneth Unruh, MD
- Mark Winston, MD

Here are some of the most common hand and wrist surgical procedures:
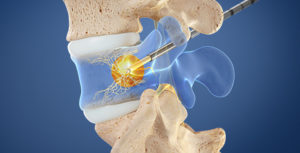
Carpal Tunnel Release
This is one of the most common hand surgeries. The goal is to relieve the pressure on the median nerve. The procedure involves cutting the transverse carpal ligament, which forms the “roof” of the carpal tunnel, to create more space for the nerve. The ligament eventually heals in a way that allows more room, preventing future compression. This procedure has a very high success rate in relieving symptoms of tingling, numbness, and weakness. It can be performed through a traditional open incision or an endoscopic, minimally invasive technique, often with a faster recovery time.
Trigger Finger A1 Pulley Release
Trigger finger occurs when the A1 pulley, a small fibrous sheath that holds the tendon close to the bone, becomes inflamed and thickens, making it difficult for the tendon to glide smoothly. This causes the characteristic “catching” or “locking” sensation. The surgical procedure, trigger finger A1 pulley release, is a simple but highly effective outpatient procedure. The surgeon makes a small incision and carefully cuts the A1 pulley, releasing the tendon. The pulley eventually heals in an open position, allowing the tendon to glide freely and restoring normal finger movement.
Wrist Arthroscopy
Arthroscopy is a minimally invasive surgical technique that uses a small camera (arthroscope) to view and operate inside a joint. For the wrist, this allows the surgeon to diagnose and treat a variety of conditions without a large incision. Wrist arthroscopy can be used to:
- Repair torn ligaments and cartilage (e.g., TFCC tears).
- Remove inflamed tissue.
- Remove or repair bone fragments.
- Debride or clean up the joint from arthritis.
This technique leads to less pain, minimal scarring, and a faster recovery compared to traditional open surgery.
Fracture Repair
A wrist fracture can be a painful and debilitating injury. While some simple fractures can be treated with a cast or splint, more complex fractures—especially those that are displaced or involve the joint—require surgery. The goal of fracture repair is to realign the broken bones and stabilize them with plates, screws, or pins. This allows the bone to heal in the correct position, restoring proper wrist alignment and function. A dedicated orthopedics specialist is essential for managing these types of injuries.

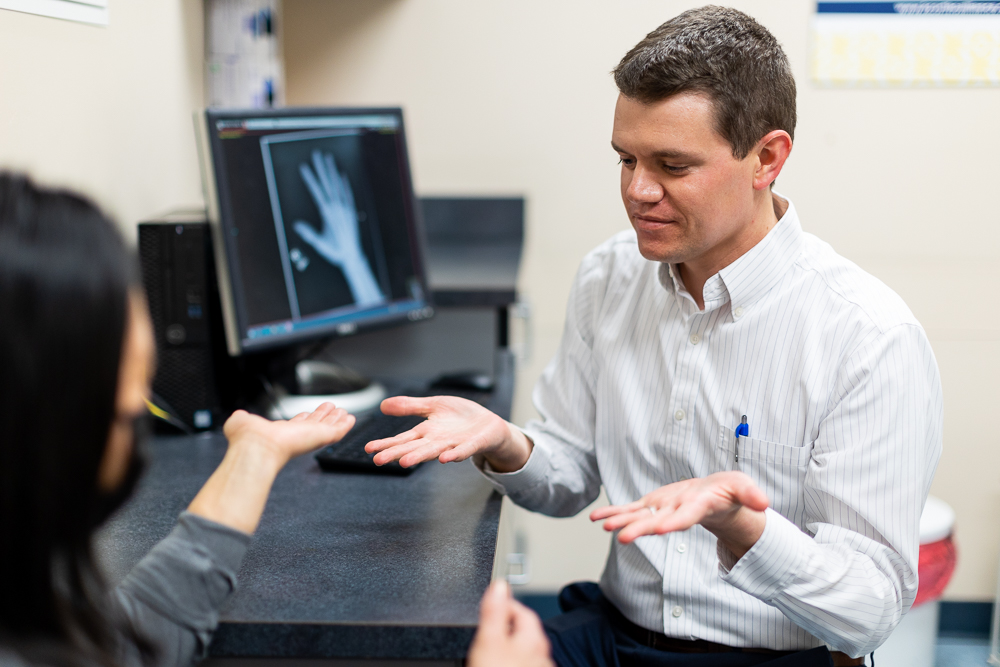
The Importance of a Comprehensive Diagnosis
Regardless of your symptoms, the most crucial first step is a proper diagnosis. Our specialists perform a thorough evaluation that includes a physical exam, a review of your medical history, and may include diagnostic imaging such as X-rays, MRI, or ultrasound. This detailed assessment allows our team to pinpoint the exact source of your hand pain or wrist pain and develop a personalized treatment plan that is right for you.
You can learn more about our specialized upper extremity services and hand and wrist care on our website. Our team includes fellowship-trained surgeons with extensive experience in the latest surgical and non-surgical techniques, ensuring you receive the highest level of care.
Take the First Step Towards a Pain-Free Future
Don’t let hand pain and wrist pain hold you back from doing the things you love. Whether your symptoms are mild or severe, there are effective solutions available. From simple therapeutic injections to advanced surgical procedures like carpal tunnel release and wrist arthroscopy, our hand and wrist team at KCOI is dedicated to helping you find relief and restore your quality of life.
We are proud to serve the Kansas City metropolitan area and surrounding communities with compassionate and expert orthopedic care. Take control of your health and schedule a consultation to discuss your treatment options.
Ready to find relief? Contact the expert orthopedics team at Kansas City Orthopedic Alliance today: Request an Appointment. Your path to recovery starts here.