Back pain affects people of all ages and can disrupt daily life, from work to the activities you enjoy. At Kansas City Orthopaedic Institute (KCOI), our specialists are here to help you understand the cause of your pain and explore personalized treatment options. In this blog, we’ll break down the most common causes and solutions to help you find lasting relief.
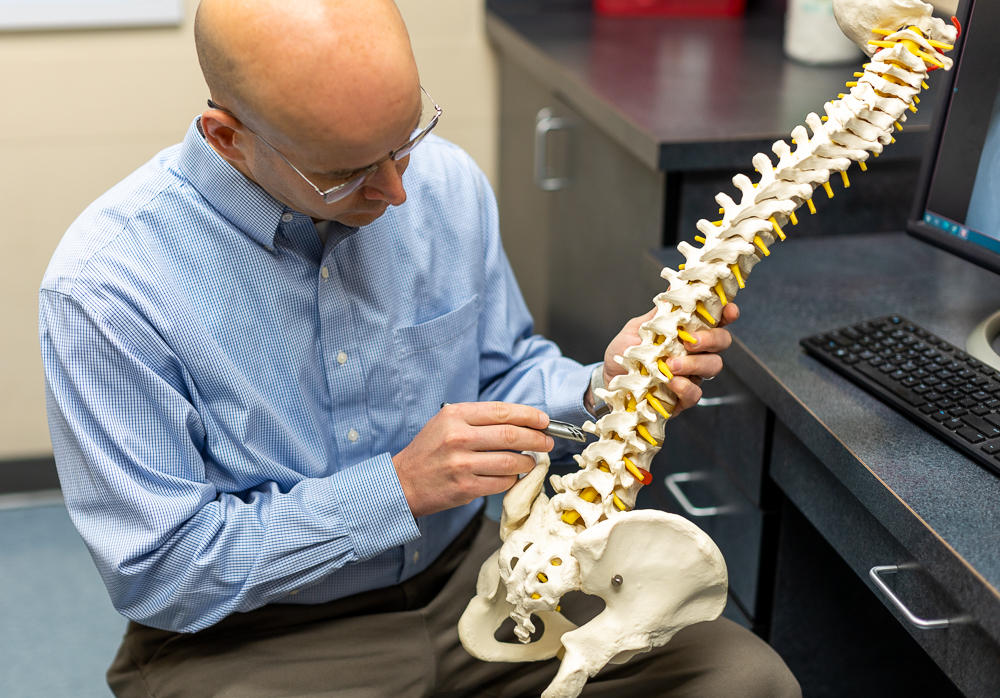
Understanding Your Back: A Marvel of Engineering
Understanding back pain starts with the spine—a complex structure of 33 vertebrae, cushioned by discs, connected by ligaments, and supported by muscles. It protects the spinal cord and enables movement. When any part is irritated or damaged, especially in the lower back, it can lead to pain, stiffness, and other symptoms.
The Many Faces of Back Pain: Common Causes
Back pain can stem from a variety of sources, ranging from simple muscle strains to more complex degenerative conditions. Recognizing the potential causes is the first step toward effective treatment.
- Muscle Strains and Ligament Sprains: Often caused by sudden awkward movements, lifting heavy objects improperly, or overstretching during physical activity. These are common injuries, especially in sports medicine.
- Disc Problems:
- Herniated or Bulging Discs: Over time, the discs can degenerate, and their soft inner material can push out (bulge) or rupture through the outer layer (herniate), pressing on nearby nerves. This is a very common cause of lower back pain and can lead to sciatica (pain radiating down the leg).
- Degenerative Disc Disease: As we age, discs naturally lose hydration and elasticity, becoming less effective shock absorbers and leading to pain and stiffness.
- Arthritis (Osteoarthritis): The cartilage cushioning the facet joints (small joints connecting the vertebrae) can wear down, leading to bone-on-bone friction, inflammation, and pain. This is a common cause of chronic back pain.
- Spinal Stenosis: A narrowing of the spinal canal, which can put pressure on the spinal cord and nerves. This often causes pain, numbness, or weakness in the legs, especially when walking.
- Spondylolisthesis: Spondylolisthesis, a condition where a vertebra slips forward, is a concern for young athletes, often stemming from spondylolysis, a stress fracture in the spine. This condition is frequently caused by repetitive twisting and hyperextension movements, making it prevalent in sports like gymnastics and football.
- Fractures: Trauma (like a fall or car accident) or weakened bones (due to osteoporosis) can lead to vertebral fractures.
- Scoliosis: An abnormal curvature of the spine, which can cause pain and imbalance, especially if severe.
- Lifestyle Factors: Poor posture, prolonged sitting, lack of exercise, obesity, and smoking can all contribute to developing or worsening back pain.
When to See an Orthopedic Specialist for Your Back Pain
Many instances of back pain are acute, meaning they come on suddenly and resolve within a few days or weeks with rest and self-care. However, certain symptoms warrant immediate attention from an orthopedic specialist. Don’t delay seeking professional help if you experience:
- Severe pain that doesn’t improve with rest.
- Pain radiating down one or both legs, especially if it extends below the knee.
- Numbness, tingling, or weakness in your legs, feet, or groin area.
- Loss of bowel or bladder control (a medical emergency).
- Unexplained weight loss accompanied by back pain.
- Fever with back pain.
- Pain that is worse at night or awakens you from sleep.
- Pain following a significant injury, such as a fall or car accident.
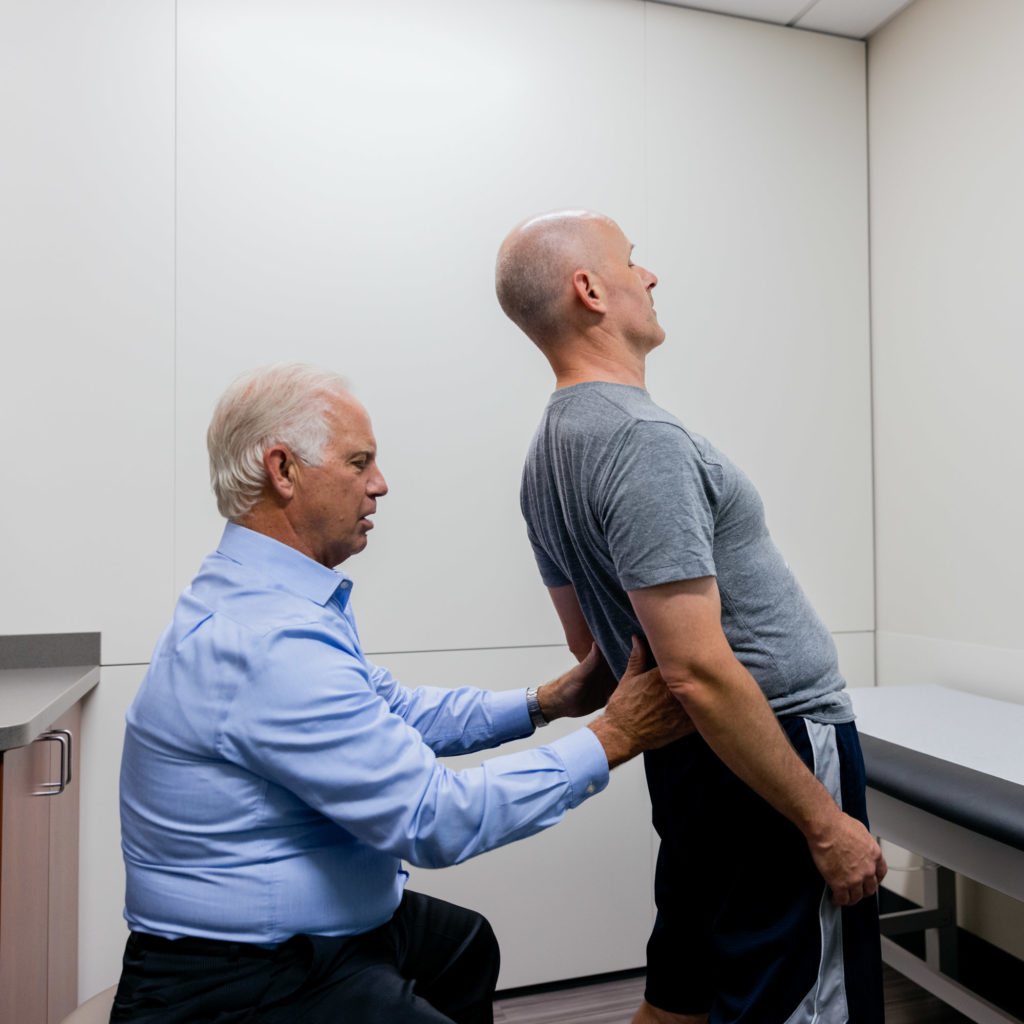
Even if your symptoms aren’t severe or alarming, if your back pain persists for more than a few weeks, interferes with your daily activities, or you find yourself constantly battling stiffness, it’s time to consult with an expert. Our team at KCOI is equipped to provide a comprehensive evaluation, diagnose the precise cause of your pain, and recommend the most effective treatment plan tailored to your needs.
Navigating Non-Surgical Treatment Options: The First Line of Defense
For most patients, the journey to relief from back pain begins with non-surgical, conservative treatments. These approaches focus on reducing pain, improving function, and empowering you to manage your condition effectively. At KCOI, we believe in a multidisciplinary approach, often combining several therapies for optimal results.
- Rest and Activity Modification: In the acute phase, brief rest can be beneficial. However, prolonged bed rest is generally discouraged. Your doctor may recommend modifying certain activities to avoid movements that aggravate your pain.
- Physical Therapy: This is often the cornerstone of non-surgical back pain treatment. A skilled physical therapist can teach you specific exercises to strengthen core muscles, improve flexibility, correct posture, and enhance body mechanics. They can also use modalities like heat, ice, ultrasound, or electrical stimulation to reduce pain and inflammation. Through our partership with KCOI Performance Rehab, there are 10 convenient outpatient locations for PT and OT.
- Medications:
- Over-the-counter pain relievers: NSAIDs (like ibuprofen or naproxen) can reduce pain and inflammation.
- Muscle relaxants: May be prescribed for muscle spasms.
- Neuropathic pain medications: For nerve-related pain.
- Injections:
- Epidural Steroid Injections: These target inflammation around irritated spinal nerves, providing significant, though often temporary, pain relief.
- Facet Joint Injections: Address pain stemming from the small facet joints in the spine.
- Nerve Blocks: Can identify the source of pain or provide sustained relief by blocking nerve signals.
- Chiropractic Care and Manual Therapy: For some types of back pain, manipulation and mobilization techniques can help restore joint motion and reduce pain.
- Alternative Therapies: Acupuncture, massage therapy, and yoga can be complementary treatments for some individuals, helping to manage pain and improve flexibility.
- Lifestyle Changes: Weight management, quitting smoking, and adopting ergonomic practices at work and home are crucial for long-term back health. Our experts can offer guidance on safe exercise and activity.
Considering Surgical Intervention: When Conservative Care Isn’t Enough
While the vast majority of back pain cases improve with conservative care, there are situations where surgery becomes a necessary and effective option. Your orthopedic surgeon at KCOI will only recommend surgery after a thorough evaluation, when non-surgical treatments have been exhausted, and if clear diagnostic evidence (like MRI scans) points to a specific anatomical problem that can be corrected surgically.
Surgical intervention for spine conditions aims to:
- Decompress Nerves: Relieve pressure on compressed nerves that are causing pain, numbness, or weakness.
- Stabilize the Spine: Fuse vertebrae together or use hardware to prevent excessive movement, particularly for instability or severe deformities.
Common types of spine surgeries for back pain include:
- Laminectomy: Often performed for herniated discs or spinal stenosis. A laminectomy involves removing part of the vertebral bone (lamina) to create more space for nerves.
- Discectomy: A discectomy removes the portion of a herniated disc that is pressing on a nerve. These can often be done with minimally invasive techniques.
- Spinal Fusion: This procedure involves permanently connecting two or more vertebrae using bone grafts and often metal hardware (screws, rods). It’s used to stabilize the spine, correct deformities, or eliminate painful motion between vertebrae, particularly in cases of severe degenerative disc disease, spondylolisthesis, or spinal instability.
- Artificial Disc Replacement: In some select cases, particularly for single-level degenerative disc disease in younger patients, the damaged disc can be removed and replaced with an artificial disc in the cervical spine, preserving motion at that spinal level.
- Vertebroplasty/Kyphoplasty: Procedures used to treat painful vertebral compression fractures, often due to osteoporosis. Bone cement is injected into the fractured vertebra to stabilize it.
The choice of surgical procedure depends entirely on the specific diagnosis, the severity of your condition, your overall health, and the recommendations of your orthopedic specialist. Our orthopedics team at KCOI prides itself on utilizing the latest surgical techniques, including minimally invasive options, to ensure the best possible outcomes for our patients.
Prevention and Proactive Spine Health
While we can’t always prevent back pain, especially from degenerative changes, adopting healthy habits can significantly reduce your risk and severity:
- Maintain a Healthy Weight: Excess weight, particularly in the abdomen, puts added strain on your lower back pain region.
- Practice Good Posture: Be mindful of how you sit, stand, and lift. When lifting, use your legs, not your back.
- Stay Active: Regular exercise strengthens core muscles that support your spine. Include activities that promote flexibility and cardiovascular health. Even gentle movement can help prevent stiffness.
- Ergonomics: Ensure your workstation is ergonomically sound to support your spine during prolonged sitting.
- Quit Smoking: Smoking reduces blood flow to the discs, accelerating their degeneration.
- Listen to Your Body: Pay attention to early warning signs of pain and take appropriate rest or modify activities.
Take Control of Your Back Health
Persistent back pain and stiffness don’t have to be your norm. Whether it’s a recent injury or chronic discomfort, our experts provide accurate diagnoses and personalized treatment to relieve pain, restore function, and improve your quality of life. Don’t let back pain hold you back. Request an appointment with one of our experienced orthopedic specialists at partner physician clinic KCOA today: Request an Appointment. Your spine health is our priority.